Meningitis DefinitionMeningitis is a rare but serious infection of the meninges. The meninges are the membranes that surround the brain and spinal cord. The most frequent causes of meningitis include viruses, bacteria, and infrequently fungus. Children are more frequently affected by viral meningitis, which is typically a less deadly type of meningitis. It may result in excruciating headaches. Viruses that dwell in feces, mouthwash, and nose fluids commonly cause viral meningitis. 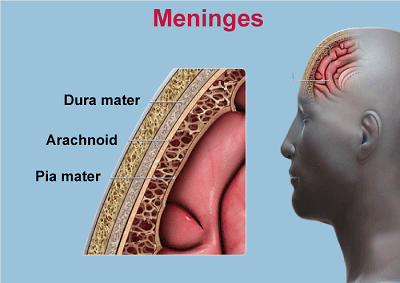 Typically, bacterial meningitis is more serious. It is brought on by germs that often cause no harm and are found in the nose and throat. However, they have the potential to enter the bloodstream and spread to the membrane that surrounds the brain, resulting in meningitis. A medical emergency is bacterial meningitis. Early identification and treatment are crucial because it can kill in a matter of hours. When should I seek Medical Attention?If your child complains of eye pain from bright lights, a persistent headache, a stiff neck, or an inexplicable fever, take them to the doctor. If you or a child displays meningococcal disease
What are the Symptoms of Meningitis?Some common symptoms are-
These are all signs of meningitis in infants and very young children:
Older children and adults who have meningitis typically exhibit the following symptoms:
The signs and symptoms don't always show up in a specific order, and some might not even show up at all. Meningitis does not always result in a rash. Not every symptom of meningitis may be included in this list of symptoms. What Causes Meningitis?Meningitis is typically transmitted from person to person through close contact, such as kissing, sneezing, coughing, and sharing of personal objects. Enteroviruses (Common stomach viruses) typically cause viral meningitis. Herpes simplex types I and II, chickenpox, measles, mumps, and lymphocytic choriomeningitis (LCM) virus are additional risk factors. Meningococcal, pneumococcal, Haemophilus influenzae type B (Hib), tuberculosis, group B streptococcus, and E. coli meningitis bacteria are all capable of causing bacterial meningitis. How is Meningitis Diagnosed?Meningitis is diagnosed with a blood test and perhaps with a lumbar puncture. In order to collect a sample of the fluid around the brain and spine, a needle is inserted into the base of the spine. To determine the sort of infection that caused the meningitis, the fluid is studied. Types of MeningitisThe leading causes of meningitis include bacterial and viral diseases. There are other additional types of meningitis. Examples include carcinomatous, which is connected to cancer, and cryptococcal, which is brought on by a fungus. These kinds are less typical. 1. Viral meningitisThe most typical type of meningitis is viral meningitis. About 52% of cases in adults and 58% in newborns are caused by viruses in the enterovirus category. These are more prevalent in the summer and in the fall, and they consist of:
Infections caused by enteroviruses account for 10 to 15 million cases per year. Annually, but only a small proportion of those who contract the infection go on to develop meningitis. Meningitis can be caused by other viruses. These consist of HIV, measles, mumps, HIV, West Nile virus, herpes viruses, and Coltivirus, which causes Colorado tick fever. Usually, viral meningitis clears up on its own. Some causes, nevertheless, do require treatment. 2. Bacterial meningitisMeningitis caused by specific bacteria is infectious and contagious. If untreated, it might be lethal. One in ten patients with bacterial meningitis die from it, and one in five suffer from severe consequences. This is still possible even with appropriate care. The most typical bacterial species that result in bacterial meningitis include-
3. Fungal meningitisA rare kind of meningitis is fungus meningitis. A fungus that affects your body causes it to spread to your brain or spinal cord through your bloodstream. A compromised immune system increases the risk of fungal meningitis. This includes those who have HIV or cancer. The fungi that cause fungal meningitis most frequently include-
4. Parasitic meningitisThis type of meningitis, which is less prevalent than viral or bacterial meningitis, is brought on by parasites that can be found in excrement, dirt, and on some types of food and animals, such as raw fish, chicken, and fruit, as well as in some snails. There are various different types of parasite meningitis. Eosinophilic meningitis (EM) is the term for it. The three primary parasites that cause EM are as follows:
No one can contract parasitic meningitis from another person. Rather, these parasites attack an animal or lurk on food that is later consumed by humans. An infection may happen if the parasite or parasite eggs are contagious when consumed. Amoebic meningitis, a very uncommon form of parasite meningitis, is a potentially fatal infection. This type is brought on by swimming in contaminated ponds, rivers, or lakes, which allows one of numerous amoeba species to enter the body through the nose. In the long run, the parasite may result in hallucinations, seizures, and other severe symptoms by destroying brain tissue. Naegleria fowleri is the species that is most frequently recognized. 5. Non-infectious meningitisMeningitis that is not contagious is not an illness. Instead, it is a form of meningitis brought on by other illnesses or medical procedures. These consist of:
Chronic MeningitisMeningitis cases that linger for more than four weeks are classified under this category. Among other things, fungus, rheumatological disorders, and cancer are among the causes of chronic meningitis. Managing rheumatoid arthritis is the primary goal of treatment for chronic meningitis. Can Meningitis be Prevented?
The best approach to prevent meningitis is to keep up with standard childhood vaccines because many of the viruses and bacteria that cause meningitis can be substantially prevented by them. There are further alternative vaccines available against various meningococcus types that can cause bacterial meningitis. Meningococcal VaccineThe best defense against meningitis illness is vaccination. Meningococcal B and ACWY vaccinations can be given starting at age 6 weeks. The meningococcal vaccine is advised for:
Complications of meningitisAfter meningitis, the majority of patients fully recover. Depending on the illness's form and intensity, some people bounce back pretty quickly while others do so more slowly. Short-term memory loss, recurrent headaches, fatigue, mood changes, and other side symptoms are common in meningitis survivors, though they typically go away over time. Meningitis can occasionally result in severe or protracted issues including a stroke, brain damage, seizures, or hearing loss. Meningitis can occasionally be lethal. Next TopicMethod Definition |